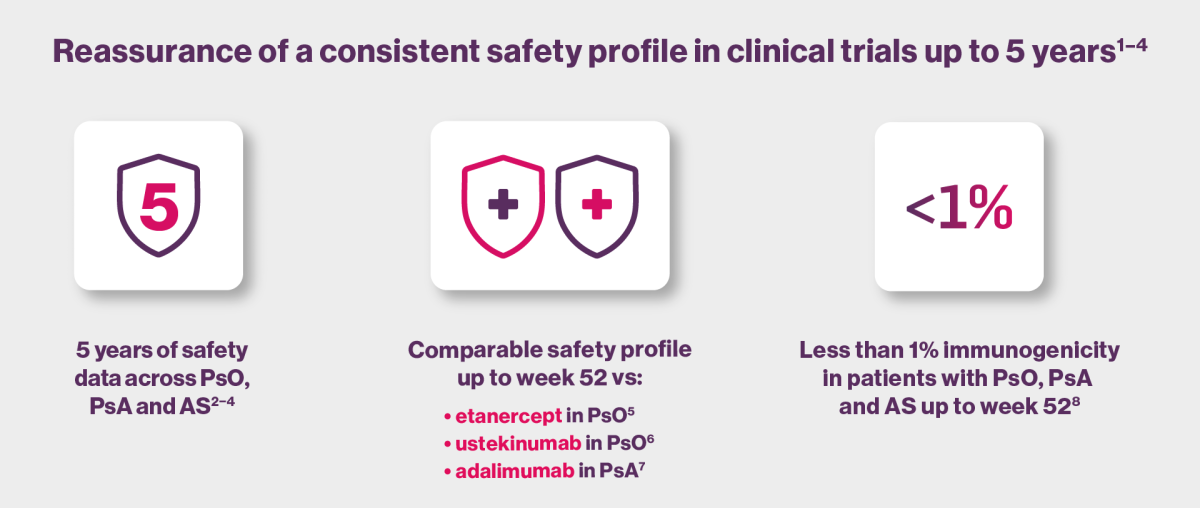
Safety profile
See the safety profile of Cosentyx across PsO, PsA and AS.
Contraindications
- Hypersensitivity to the active substance or to any of the excipients
- Clinically important, active infection, e.g. active tuberculosis
Special warnings and precautions for use
Infections
Cosentyx has the potential to increase the risk of infections. Serious infections have been observed in patients receiving Cosentyx. Caution should be exercised when considering the use of Cosentyx in patients with a chronic infection or a history of recurrent infection. Patients should be instructed to seek medical advice if signs or symptoms suggestive of an infection occur.
No increased susceptibility to tuberculosis was reported from clinical studies. However, Cosentyx should not be given to patients with active tuberculosis. Anti-tuberculosis therapy should be considered prior to initiation of Cosentyx in patients with latent tuberculosis.
Inflammatory bowel disease (including Crohn’s disease and ulcerative colitis)
Cases of new or exacerbations of inflammatory bowel disease have been reported with Cosentyx®. Cosentyx is not recommended in patients with inflammatory bowel disease. If a patient develops signs and symptoms of inflammatory bowel disease or experiences an exacerbation of pre-existing inflammatory bowel disease, Cosentyx should be discontinued and appropriate medical management should be initiated.
Hypersensitivity reactions
Rare cases of anaphylactic reactions and angioedema have been observed in patients receiving Cosentyx. If an anaphylactic reaction, angioedema or other serious allergic reactions occur, administration of Cosentyx should be discontinued immediately and appropriate therapy initiated.
Vaccinations
Live vaccines should not be given concurrently with Cosentyx. Patients receiving Cosentyx may receive concurrent inactivated or non-live vaccinations. Prior to initiating therapy with Cosentyx, it is recommended that paediatric patients receive all age-appropriate immunisations as per current immunisation guidelines.
Concomitant immunosuppressive therapy
In psoriasis studies, the safety and efficacy of Cosentyx in combination with immunosuppressants, including biologics, or phototherapy have not been evaluated. Cosentyx was administered concomitantly with methotrexate (MTX), sulfasalazine and/or corticosteroids in arthritis studies
Hepatitis B reactivation
Hepatitis B virus reactivation can occur in patients treated with Cosentyx. In accordance with clinical guidelines for immunosuppressants, testing patients for HBV infection is to be considered before initiating treatment with Cosentyx.. Patients with evidence of positive HBV serology should be monitored for clinical and laboratory signs of HBV reactivation during Cosentyx. treatment. If reactivation of HBV occurs while on Cosentyx., discontinuation of the treatment should be considered, and patients should be treated according to clinical guidelines.
Latex-sensitive individuals
The removable cap of the Cosentyx pre-filled pen contains a derivative of natural rubber latex.
Tabulated list of adverse reactions from the SmPC8
| System Organ Class | Frequency† | Adverse reaction |
|---|---|---|
| Infections and infestations | Very common | Upper respiratory tract infections |
| Common | Oral herpes | |
| Tinea pedis | ||
| Uncommon | Oral candidiasis | |
| Otitis externa | ||
| Lower respiratory tract infections | ||
| Not known | Mucosal and cutaneous candidiasis (including oesophageal candidiasis) | |
| Blood and lymphatic system disorders | Uncommon | Neutropenia |
| Immune system disorders | Rare | Anaphylactic reactions |
| Angioedema | ||
| Nervous system disorders | Common | Headache |
| Eye disorders | Uncommon | Conjunctivitis |
| Respiratory, thoracic and mediastinal disorders | Common | Rhinorrhoea |
| Gastrointestinal disorders | Common | Diarrhoea |
| Nausea | ||
| Uncommon | Inflammatory bowel disease | |
| Skin and subcutaneous tissue disorders | Common | Eczema |
| Uncommon | Urticaria | |
| dyshidrotic eczema | ||
| Rare | Exfoliative dermatitis‡ | |
| Hypersensitivity vasculitis | ||
| General disorders and administration site conditions | Common | Fatigue |
*Placebo-controlled, phase III clinical studies in PsO, PsA, AS and nr-axSpA. Some of the doses and dose regimes used in these studies are not approved for use.
AEs captured include patients exposed to Cosentyx 300 mg, 150 mg, 75 mg or placebo up to 12 weeks (PsO) or 16 weeks (PsA, AS and nr-axSpA) of treatment duration; please refer to the Cosentyx SmPC for full prescribing information.
†Corresponding frequency category for each adverse drug reaction is based on the following convention: very common (≥1/10); common (≥1/100 to <1/10); uncommon (≥1/1,000 to <1/100); rare (≥1/10,000 to <1/1,000); very rare (<1/10,000); and not known (cannot be estimated from the available data).
‡Cases were reported in patients with psoriasis diagnosis.
Safety data and selected AEs from 21 clinical trials1
| PsO studies Any Cosentyx (N=5181) |
PsA studies Any Cosentyx (N=1380) |
AS studies Any Cosentyx (N=794) |
|
| Total exposure, patient-years | 10,416.9 | 3866.9 | 1943.1 |
|---|---|---|---|
| Min–max exposure (days) | 1−1825 | 8−1827 | 1−1530 |
| Death, n (%) | 9 (0.2) | 11 (0.8) | 5 (0.6) |
| Discontinuations due to AEs, n (%) | 331 (6.4) | 104 (7.5) | 58 (7.3) |
| EAIR per 100 patient-years (95% CI) | |||
| Any AE | 204.4 (198.4, 210.5) | 147.0 (138.9, 155.5) | 140.1 (129.8, 151.0) |
| Any serious AE | 6.9 (6.3, 7.4) | 7.9 (7.0, 8.9) | 6.3 (5.2, 7.6) |
| Most common AEs* | |||
| Viral URTI† | 21.0 (19.9, 22.0) | 12.1 (10.9, 13.4) | 9.8 (8.4, 11.5) |
| Headache | 6.2 (5.8, 6.8) | 3.8 (3.2, 4.5) | 5.3 (4.3, 6.5) |
| Diarrhoea | 3.8 (3.4, 4.2) | 3.7 (3.1, 4.4) | 5.2 (4.2, 6.4) |
| URTI | 5.4 (4.9, 5.9) | 9.1 (8.1, 10.2) | 5.2 (4.2, 6.4) |
| Selected AEs | |||
| Serious infections‡ | 1.4 (1.2, 1.6) | 1.9 (1.5, 2.4) | 1.2 (0.8, 1.8) |
| Candida infections§ | 2.2 (1.9, 2.5) | 1.5 (1.1, 2.0) | 0.7 (0.4, 1.2) |
| IBD¶ | 0.01 (0.00, 0.05) | 0.05 (0.01, 0.2) | 0.1 (0.0, 0.3) |
| Crohn’s disease¶ | 0.05 (0.02, 0.1) | 0.08 (0.02, 0.2) | 0.4 (0.2, 0.8) |
| Ulcerative colitis¶ | 0.1 (0.07, 0.2) | 0.08 (0.02, 0.2) | 0.2 (0.1, 0.5) |
| MACE| | 0.3 (0.2, 0.5) | 0.4 (0.3, 0.7) | 0.6 (0.3, 1.1) |
| Neutropenia¶ | 0.3 (0.2, 0.4) | 0.2 (0.1, 0.4) | 0.5 (0.3, 1.0) |
| Uveitis¶ | 0.02 (0.0, 0.07) | 0.1 (0.0, 0.2) | 1.4 (0.9, 2.0) |
| Malignancy# | 0.8 (0.6, 1.0) | 1.1 (0.8, 1.5) | 0.5 (0.2, 0.9) |
Adverse events were reported as exposure adjusted incident rates (EAIRs) per 100 patient-years. Analyses included all patients who received one or more doses of Cosentyx. Approximation was not done if EAIR is less than 0.1.
Some of the doses and dose regimes used in these studies are not approved for use (including 10 mg/kg intravenous loading and 75 mg subcutaneous dose). Individual patient dosing may vary - please consult the Cosentyx SmPC for full prescribing information, available at www.medicines.ie
*AEs in the secukinumab group that occurred with an incidence rate >5.0 per 100 patient-years during the entire safety period in any of the pooled groups.
†Includes cases of common cold (low-level term)
‡Values are based on system organ class: infections and infestations
§Values are based on the high-level term
¶Values are based on the preferred term
|Values are based on Novartis Medical Dictionary for Regulatory Activities query, which comprises (1) any myocardial infarction, (2) any cardiovascular accident, and (3) all other cardiovascular events that are fatal, out of a listing of 2200+ terms
#Values are based on standardized MedDRA query
Table adapted from Deodhar et al. 2019.1
From an extension to the SCULPTURE study2
| Cosentyx 300 mg | |||||
| Year 1 N=168 |
Year 2 N=168 |
Year 3 N=157 |
Year 4 N=142 |
Year 5 N=134 |
|
| n (incidence rate per 100 subject-years) | |||||
| Duration of exposure (patient-years)* | 168.0 | 162.8 | 148.8 | 136.5 | 142.0 |
|---|---|---|---|---|---|
| All AEs | 131 (204.6) | 126 (166.3) | 109 (139.2) | 91 (118.5) | 77 (87.2) |
| All non-fatal SAEs | 14 (8.8) | 11 (6.9) | 13 (9.1) | 13 (10.1) | 11 (8.0) |
| Death | 0 | 0 | 0 | 0 | 1 (0.7)† |
| Most frequent AEs | |||||
| Nasopharyngitis | 30 (20.1) | 27 (18.1) | 25 (18.8) | 17 (13.5) | 15 (11.1) |
| Hypertension | 11 (6.8) | 8 (5.1) | 3 (2.0) | 7 (5.3) | 5 (3.6) |
| Back pain | 7 (4.3) | 9 (5.7) | 9 (6.2) | 3 (2.2) | 3 (2.1) |
| URTI | 12 (7.5) | 11 (7.1) | 5 (3.5) | 5 (3.8) | 5 (3.6) |
| Headache | 10 (6.2) | 7 (4.4) | 4 (2.7) | 3 (2.2) | 1 (0.7) |
| Selected rare AEs | |||||
| Opportunistic infections (other than TB and candidiasis) | 0 | 0 | 0 | 0 | 0 |
| TB | 0 | 0 | 0 | 0 | 0 |
| Candida infections | |||||
| Vulvovaginal candidiasis | 3 (1.8) | 3 (1.9) | 1 (0.7) | 0 | 0 |
| Oral candidiasis | 0 | 1 (0.6) | 0 | 1 (0.7) | 1 (0.7) |
| Neutropenia | 0 | 0 | 0 | 0 | 0 |
| MACE | 0 | 0 | 0 | 1 (0.7) | 1 (0.7)† |
| Crohn’s disease | 0 | 0 | 0 | 0 | 0 |
| Ulcerative colitis | 0 | 2 (1.2)‡ | 1 (0.7) | 0 | 0 |
| Malignant or unspecified tumours (excluding NMSC) | 0 | 2 (1.2)§ | 0 | 0 | 1 (0.7)¶ |
Only subjects who completed the SCULPTURE core study and continued into the extension are included in this analysis. A subject with multiple occurrences of the same AE in a one-year interval was counted only once, while a subject with multiple occurrences of the same AE in different year intervals was counted for each year.
*Patient exposure is calculated as a sum of individual subject durations in days divided by 365 for each interval.
†Death was due to MACE, which was not considered by the investigators to be related to study drug; patient had ≥2 pre-existing MACE risk factors.
‡Of the two cases of ulcerative colitis in year 2, one case was an exacerbation of previously existing ulcerative colitis; the exposure-adjusted incidence rate for new-onset ulcerative colitis cases for the entire study duration (5 years) was 0.27.
§One case of cholangiocarcinoma, one case of invasive ductal breast carcinoma.
¶One case of breast cancer.
Table adapted from Bissonnette et al. 2018.2
FIXTURE double-blind RCT5
| Any Cosentyx 300mg (N=467) |
Etanercept (N=323) |
Placebo (N=327)† |
|
| Exposure to study treatment, days* | 320.7±75.3 | 331.9±89.7 | 95.3±61.0 |
|---|---|---|---|
| no. of patients with event (no. of cases per 100 patient-years) | |||
| Any adverse event | 376 (252.0) | 253 (243.4) | 168 (329.7) |
| Death | 0 | 0 | 0 |
| Non-fatal serious adverse event | 27 (6.8) | 20 (7.0) | 7 (8.3) |
| Discontinuation due to adverse event‡ | 14 | 12 | 3 |
| Infection or infestation | 269 (105.4) | 170 (91.4) | 65 (89.5) |
| Common adverse events§ | |||
| Nasopharyngitis | 122 (35.2) | 86 (35.7) | 26 (32.8) |
| Headache | 58 (15.7) | 40 (15.2) | 24 (29.6) |
| Diarrhoea | 38 (9.9) | 22 (7.9) | 7 (8.4) |
| Pruritus | 16 (4.0) | 16 (5.7) | 11 (13.2) |
| Arthralgia | 24 (6.0) | 23 (8.2) | 10 (12.1) |
| URTI | 26 (6.6) | 18 (6.4) | 3 (3.5) |
| Back pain | 31 (7.9) | 26 (9.3) | 6 (7.1) |
| Cough | 30 (7.6) | 12 (4.2) | 4 (4.8) |
| Hypertension | 20 (5.0) | 14 (4.9) | 4 (4.7) |
| Nausea | 11 (2.7) | 7 (2.4) | 7 (8.3) |
| Oropharyngeal pain | 25 (6.3) | 10 (3.5) | 7 (8.3) |
Data from the 150 mg group have not been presented here, as this dose is not approved for use in PsO. Individual patient dosing may vary - please consult the Prescribing Information for full details or refer to the Cosentyx SmPC for full prescribing information.
*Plus-minus values are means ± SDs.
†Placebo patients not achieving PASI 75 at week 12, underwent randomisation to Cosentyx 150 mg or 300 mg. In this 52 week analysis, the placebo group includes all patients who received placebo during the induction period, including 16 patients who achieved PASI 75 at week 12 and continued to receive placebo during maintenance period (week 13 to week 52).
‡Exposure-adjusted incidence rates were not calculated for discontinuations due to adverse events.
§Events that had an incidence rate of at least 5.0 cases per 100-patient years in the combined secukinumab groups during the entire treatment period.
Table adapted from Langley et al. 2014.5
CLEAR double-blind RCT6
| Variable | Cosentyx 300 mg (N=335) n (incidence rate per 100 subject-years) [95% CI] |
Ustekinumab (N=336) n (incidence rate per 100 subject-years) [95% CI] |
|---|---|---|
| Any AE | 286 (280.9) [249.3–315.4] | 278 (250.1) [221.6–281.3] |
| Serious AEs | 30 (9.6) [6.5–13.7] | 26 (8.5) [5.5–12.4] |
| Death | 0 | 1 |
| Discontinued treatment due to AE | 10 | 9 |
| System organ class | ||
| Infections and infestations* | 197 (98.4) [85.1–113.1] | 194 (95.8) [82.8–110.3] |
| Most frequent individual AEs† | ||
| Nasopharyngitis | 77 (27.1) [21.4–33.8] | 83 (31.0) [24.7–38.5] |
| Headache | 40 (13.5) [9.7–18.4] | 41 (14.2) [10.2–19.3] |
| Upper respiratory tract infection | 31 (10.1) [6.9–14.3] | 30 (9.9) [6.7–14.2] |
| Arthralgia | 25 (8.1) [5.3–12.0] | 28 (9.2) [6.1–13.3] |
| Diarrhoea | 23 (7.5) [4.7–11.2] | 24 (7.9) [5.1–11.8] |
| Back pain | 22 (7.1) [4.4–10.7] | 26 (8.5) [5.6–12.5] |
Individual patient dosing may vary - please consult the Cosentyx SmPC for full prescribing information, available at www.medicines.ie.
*Primary system organ class AE.
†Preferred term AEs occurring at an incidence rate per 100 subject-years ≥5.0 in the treatment groups; sorted by descending order of incidence in the secukinumab treatment group.
Table adapted from Blauvelt et al. 2017.6
EXCEED double-blind RCT7*
| Cosentyx 300 mg SC (N=426) |
Adalimumab 40 mg SC (N=427) |
|
| Duration of exposure, mean days (SD) | 351.7 (77.9) | 332.9 (94.2) |
|---|---|---|
| Number of patients with any AE, n (%) | 330 (77) | 338 (79) |
| Number of patients with serious or other significant events | ||
| Death, n† | 1 | 0 |
| Non-fatal SAE, n (%) | 32 (8) | 28 (7) |
| Discontinued study treatment due to AE, n (%) | 17 (4) | 32 (7) |
| AEs of interest, n (%) | ||
| Infections and infestations | 237 (56) | 234 (55) |
| Serious infections | 7 (2) | 6 (1) |
| Candida infections (high-level term) | 16 (4) | 7 (2) |
| Viral infectious disorders | 66 (15) | 65 (15) |
| Injection-site reactions | 17 (4) | 47 (11) |
| Hypersensitivity | 39 (9) | 60 (14) |
| MACE | 2 (<1) | 0 |
| IBD‡ | 2 (<1) | 0 |
| Crohn’s disease | 1‡ (<1) | 0 |
| Ulcerative colitis | 2‡ (<1) | 0 |
| Malignancies | 2 (<1) | 3 (1) |
| Most frequent TEAEs, n (%) | ||
| Nasopharyngitis | 81 (19) | 80 (19) |
| Upper respiratory tract infection | 41 (10) | 49 (11) |
| Headache | 35 (8) | 32 (7) |
| Diarrhoea | 31 (7) | 35 (8) |
| Hypertension | 27 (6) | 23 (5) |
| Oropharyngeal pain | 25 (6) | 15 (4) |
| Psoriasis | 24 (6) | 25 (6) |
| Arthralgia | 23 (5) | 29 (7) |
| Psoriatic arthropathy | 20 (5) | 26 (6) |
| Back pain | 14 (3) | 31 (7) |
| Bronchitis | 14 (3) | 23 (5) |
| Rash | 8 (2) | 21 (5) |
| Injection-site reactions | 4 (1) | 28 (7) |
Individual patient dosing may vary - the Cosentyx SmPC for full prescribing information, available at www.medicines.ie.
*Weeks 48 and 50 were the last dosing visit for Cosentyx 300 mg SC and adalimumab 40 mg SC, respectively.
†53-year-old male patient entered the study without any reported medical history or active medical condition. On study day 85, patient had severe abdominal pain considered as a serious event, which led to discontinuation of secukinumab and study. Colon cancer was diagnosed subsequently, with fatal outcome on day 146. Event was assessed as not related to study drug by the investigator.
‡Same patient was diagnosed with both Crohn’s and ulcerative colitis.
Table adapted from McInnes et al. 2020.7
AE, adverse event; AS, ankylosing spondylitis; CI, confidence interval; CRP, C-reactive protein; CV, cardiovascular; CVA, cardiovascular accident; DMARD, disease-modifying anti-rheumatic drug; EAIR, exposure-adjusted incidence rate; IBD, inflammatory bowel disease; MACE, major adverse cardiovascular event; MedDRA, Medical Dictionary for Regulatory Activities; MI, myocardial infarction; MTX, methotrexate; N, number of patients in the analysis; n, number of patients with a response; NMSC, non-melanoma skin cancer; nr-axSpA, non-radiographic axial spondyloarthritis; PASI, psoriasis area severity index; PsA, psoriatic arthritis; PsO, plaque psoriasis; RCT, randomised controlled trial; SAE, serious adverse event; SC, subcutaneous; SD, standard deviation; SmPC, summary of product characteristics; TEAE, treatment-emergent adverse event; TB, tuberculosis; TNF, tumour necrosis factor; URTI, upper respiratory tract infection.
References
- Deodhar A et al. Arthritis Res Ther 2019;21:111.
- Bissonnette R et al. J Eur Acad Dermatol Venereol 2018;32:1507–1514.
- Mease PJ et al. ACR Open Rheum 2020;2:18–25.
- Baraliakos X et al. RMD Open 2019;5:e001005.
- Langley RG et al. N. Engl J Med 2014;371:326–338.
- Blauvelt A et al. J Am Acad Dermatol 2017;76:60–69.
- McInnes IB et al. Lancet 2020;395(10235):1496–1505.
- Cosentyx (secukinumab) Summary of Product Characteristics. Available at www.medicines.ie. Accessed November 2024
