ENTRESTO is indicated in adult patients for the treatment of symptomatic chronic heart failure with reduced ejection fraction.1,2
For full safety information, please refer to the Summary of Product Characteristics.1
On this page you can find information on specific adverse events.
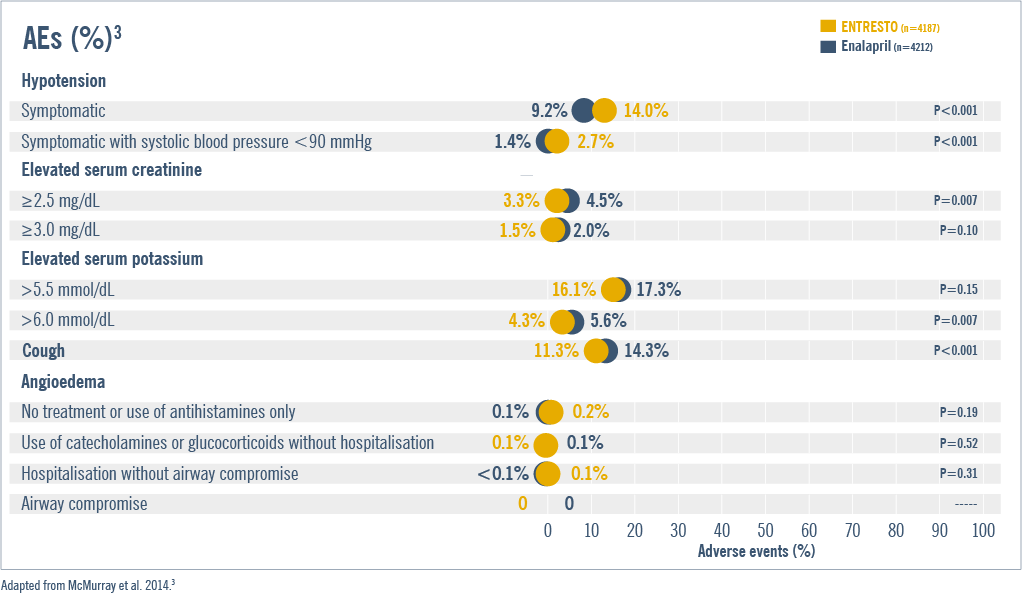
ENTRESTO demonstrates a comparable safety profile to ACEi (enalapril)1–5
ENTRESTO generally demonstrated comparable safety and tolerability vs ACEi (enalapril)1–3

The most commonly reported AEs with ENTRESTO were hypotension (17.6%) , hyperkalaemia (11.6%) and renal impairment (10.1%)1–3

Angioedema was reported in patients treated with ENTRESTO (0.5%)1,2

Fewer patients taking ENTRESTO discontinued therapy due to an AE during the double-blind period: 10.7% vs 12.3% with enalapril (P=0.03)1,3

While more patients experience symptomatic hypotension with ENTRESTO than with ACEi (enalapril), there was no increase in the discontinuation rate due to hypotension-related effects (0.9% vs 0.7%; P=0.38)3
PARADIGM-HF: N=8442, multinational, randomised, double-blind trial comparing ENTRESTO to enalapril in symptomatic (NYHA Class II-IV) HFrEF patients (LVEF ≤40%, amended later to ≤35%). The primary outcome was a composite of death from cardiovascular causes or hospitalisation for heart failure, but the trial was designed to detect a difference in the rates of death from cardiovascular causes. Secondary outcomes included time to death from any cause, the change from baseline to 8 months in the clinical summary score on the Kansas City Cardiomyopathy Questionnaire (KCCQ) the time to new onset of atrial fibrillation, and the time to the first occurrence of a decline in renal function. Adjudication of these outcomes was carried out in a blinded fashion by a clinical-end-points committee according to prespecified criteria.3
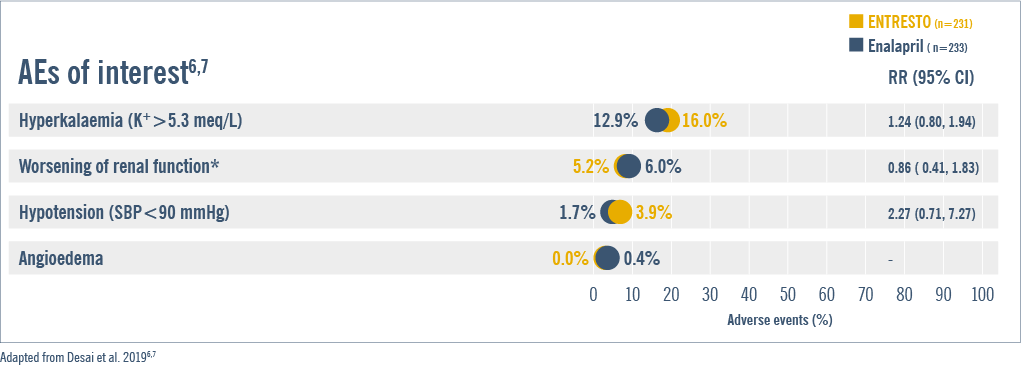

The most frequent AEs were hyperkalaemia (16.0%), worsening of renal function (5.2%), hypotension (3.9%), and angioedema (0.0%)6,7
EVALUATE-HF: N=465, multicentre, randomised, double-blind, parallel group, trial comparing ENTRESTO vs enalapril on changes in central aortic stiffness in patients with HFrEF over 12 weeks. The primary outcome was the between-group difference in change in aortic characteristic Zc from baseline to Week 12.† The secondary outcomes included: change from baseline to Week 12 in NT-proBNP, and predefined cardiac remodelling measures including, LVEF, Global Longitudinal Strain, LAVi, e’ velocity, mitral E/e’ ratio, LVESVi, LVEDVi, and Ea/Ees ratio.6
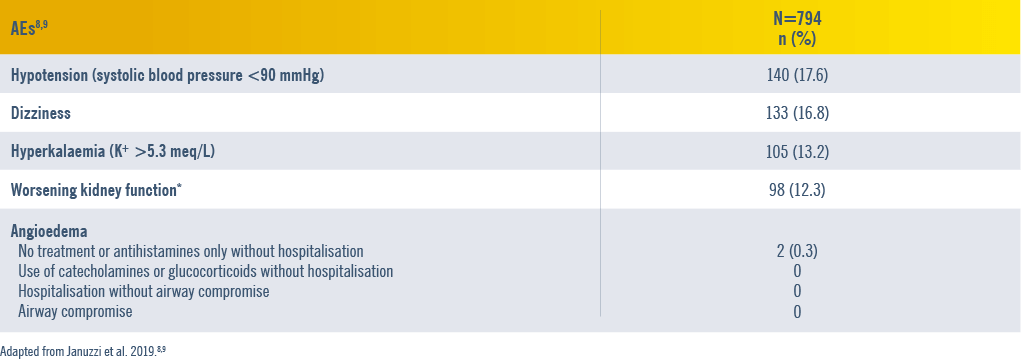

The most frequent AEs were hypotension (17.6%), dizziness (16.8%), hyperkalaemia (13.2%), and worsening kidney function (12.3%)8
PROVE-HF: N=794, phase IV, single-arm, multicentre, open-label trial in the United States conducted. 654 (82.4%) patients completed the 52-week study. It evaluated the effects of ENTRESTO on biomarkers, cardiac remodelling, and patient-reported outcomes in HFrEF. The primary outcome was the correlation between changes in NT-proBNP concentration and cardiac remodelling measures including, LVEF, LAVi, E/e’ ratio, LVESVi and LVEDVi.8
ENTRESTO had a comparable safety and tolerability profile vs ACEi (enalapril)4,10
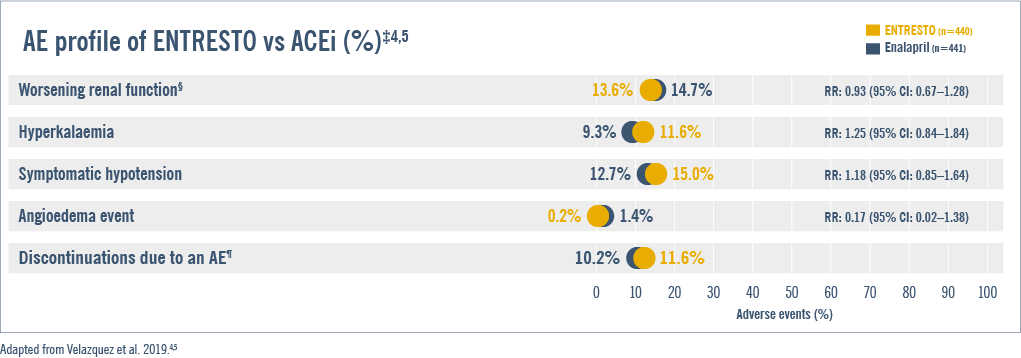

Early ENTRESTO initiation was well tolerated and showed a comparable safety profile shortly after a stabilised ADHF episode4
PIONEER-HF: N=881, prospective, multicentre, double-blind, randomised, active-controlled trial designed to assess, over an 8-week period, the safety, tolerability, and efficacy of in-hospital initiation of ENTRESTO, compared with enalapril, in adult patients in the United States with chronic HFrEF (EF ≤40% and NT-pro BNP ≥1600 pg/mL or BNP ≥400 pg/mL) haemodynamically stabilised during hospitalisation for an episode of ADHF.4 The primary endpoint was time-averaged proportional change in NT-proBNP concentration from baseline through Weeks 4 and 8. Secondary biomarker outcomes included time- averaged proportional changes in the high sensitivity troponin T and BNP concentration, and ratio of BNP to NT-proBNP. Key safety outcomes were incidences of worsening renal function, hyperkalaemia, symptomatic hypotension and angioedema. The exploratory endpoints included the outcome of a composite of serious clinical events including death, rehospitalisation for HF, implantation of a LV device, and inclusion on the list of patients eligible for heart transplantation.4
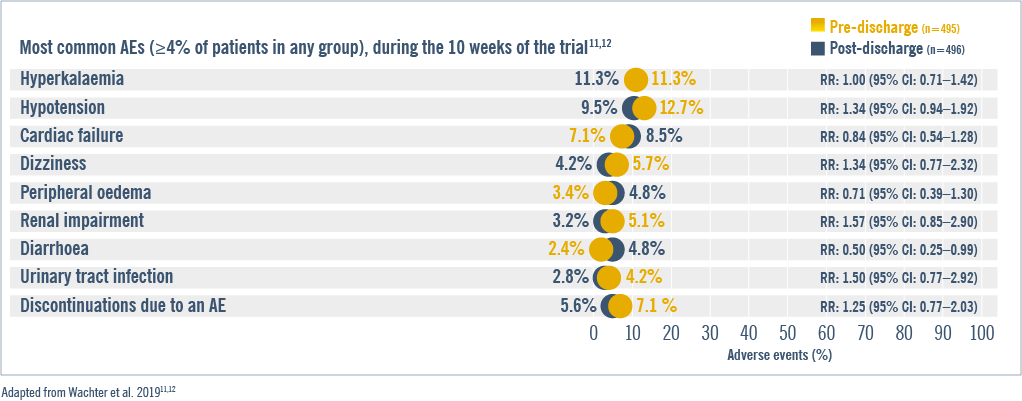

ENTRESTO demonstrated comparable safety profile when initiated either before or shortly after discharge in chronic HFrEF patients who had been haemodynamically stabilised from an episode of ADHF8,11
TRANSITION: N=1002, 10-week, randomised, parallel, open-label study comparing pre- vs post-discharge (within 1–14 days) initiation of ENTRESTO in patients with chronic HFrEF (NYHA Class II-IV HF, LVEF ≤40%) following haemodynamic stabilisation after an episode of ADHF. The primary endpoint evaluated the proportion of patients in the pre- vs post-discharge treatment initiation groups who achieved the target ENTRESTO dose of 200 mg BID at the end of Week 10 after randomisation. The secondary endpoints assessed the proportion of patients who achieved and maintained a dose of 100mg or 200mg BID for at least 2 weeks leading to Week 10, any dose of ENTRESTO for at least 2 weeks leading to Week 10 randomisation and discontinuation due to Adverse events. Key exploratory endpoints included levels of NT-proBNP, heart failure signs, time to first rehospitalisation, patients re-hospitalised, median ENTRESTO dose during 10-weeks and mean time to ENTRESTO initiation.11
Contraindications:1
- Hypersensitivity to the active substances or to any of the excipients listed in the SmPC
- Concomitant use with ACEi. ENTRESTO should not be administered until 36 hours after discontinuing ACEi therapy
- Known history of angioedema related to previous ACEi or ARB therapy
- Hereditary or idiopathic angioedema
- Concomitant use with aliskiren-containing medicinal products in patients with diabetes mellitus or in patients with renal impairment (eGFR <60 mL/min/1.73m2)
- Severe hepatic impairment, biliary cirrhosis and cholestasis
- Second and third trimesters of pregnancy
Special warnings and precautions for use1
Dual blockade of the renin-angiotensin-aldosterone system (RAAS)
- The combination of ENTRESTO with an ACEi is contraindicated due to the increased risk of angioedema. ENTRESTO must not be initiated until 36 hours after taking the last dose of ACEi therapy. If treatment with ENTRESTO is stopped, ACEi therapy must not be initiated until 36 hours after the last dose of ENTRESTO
- The combination of ENTRESTO with direct renin inhibitors such as aliskiren is not recommended. The combination of ENTRESTO with aliskiren-containing products is contraindicated in patients with diabetes mellitus or in patients with renal impairment (eGFR <60 mL/min/1.73m2)
- ENTRESTO contains valsartan, and therefore should not be co-administered with another ARB-containing product
Hypotension
- Treatment should not be initiated unless SBP is ≥100 mmHg. Patients with SBP <100 mmHg were not studied. Cases of symptomatic hypotension have been reported in patients treated with ENTRESTO during clinical studies, especially in patients ≥65 years old, patients with renal disease and patients with low SBP (<112 mmHg)
- When initiating therapy or during dose titration with ENTRESTO, blood pressure should be monitored routinely. If hypotension occurs, temporary down-titration or discontinuation of ENTRESTO is recommended. Dose adjustment of diuretics, concomitant antihypertensives and treatment of other causes of hypotension (e.g. hypovolaemia) should be considered
- Symptomatic hypotension is more likely to occur if the patient has been volume-depleted, e.g. by diuretic therapy, dietary salt restriction, diarrhoea or vomiting. Sodium and/or volume depletion should be corrected before starting treatment with ENTRESTO, however, such corrective action must be carefully weighed against the risk of volume overload
Renal Impairment
- Evaluation of patients with heart failure should always include assessment of renal function. Patients with mild and moderate renal impairment are more at risk of developing hypotension. There is very limited clinical experience in patients with severe renal impairment (estimated GFR <30 mL/min/1.73m2) and these patients may be at greatest risk of hypotension. There is no experience in patients with end-stage renal disease and use of ENTRESTO is not recommended
Worsening renal function
- Use of ENTRESTO may be associated with decreased renal function. The risk may be further increased by dehydration or concomitant use of Non-Steroidal Anti-Inflammatory Drugs (NSAIDs). Down-titration should be considered in patients who develop a clinically significant decrease in renal function
Hyperkalaemia
- Treatment should not be initiated if the serum potassium level is >5.4 mmol/l. Use of ENTRESTO may be associated with an increased risk of hyperkalaemia, although hypokalaemia may also occur. Monitoring of serum potassium is recommended, especially in patients who have risk factors such as renal impairment, diabetes mellitus or hypoaldosteronism or who are on a high potassium diet or on mineralocorticoid antagonists. If patients experience clinically significant hyperkalaemia adjustment of concomitant medicinal products or temporary down–titration or discontinuation is recommended. If serum potassium level is >5.4 mmol/L, discontinuation should be considered
Angioedema
- Angioedema has been reported in patients treated with ENTRESTO. If angioedema occurs, ENTRESTO should be immediately discontinued and appropriate therapy and monitoring should be provided until complete and sustained resolution of signs and symptoms has occurred. It must not be re-administered. In cases of confirmed angioedema where swelling has been confined to the face and lips, the condition has generally resolved without treatment, although antihistamines have been useful in relieving symptoms
- Angioedema associated with laryngeal oedema may be fatal. Where there is involvement of the tongue, glottis or larynx likely to cause airway obstruction, appropriate therapy, e.g. adrenaline solution 1 mg/1 mL (0.3–0.5 mL), and/or measures necessary to ensure a patent airway, should be promptly administered
- Patients with a prior history of angioedema were not studied. As they may be at higher risk for angioedema, caution is recommended if ENTRESTO is used in these patients. ENTRESTO is contraindicated in patients with a known history of angioedema related to previous ACEi or ARB therapy or with hereditary or idiopathic angioedema
- Black patients have an increased susceptibility to develop angioedema
Patients with renal artery stenosis
- ENTRESTO may increase blood urea and serum creatinine levels in patients with bilateral or unilateral renal artery stenosis
- Caution is required in patients with renal artery stenosis and monitoring of renal function is recommended
Patients with NYHA functional classification IV
- Caution should be exercised when initiating ENTRESTO in patients with NYHA functional classification IV due to limited clinical experience in this population
B-type natriuretic peptide (BNP)
- BNP is not a suitable biomarker of heart failure in patients treated with ENTRESTO because it is a neprilysin substrate
Patients with hepatic impairment
- There is limited clinical experience in patients with moderate hepatic impairment (Child-Pugh B classification) or with AST/ALT values more than twice the upper limit of the normal range. In these patients, exposure may be increased and safety is not established. Caution is therefore recommended when using it in these patients
- ENTRESTO is contraindicated in patients with severe hepatic impairment, biliary cirrhosis or cholestasis (Child-Pugh C classification)
Psychiatric disorders
- Psychiatric events such as hallucinations, paranoia and sleep disorders, in context of psychotic events, have been associated with ENTRESTO use. If a patient experiences such events, discontinuation of ENTRESTO treatment should be considered
ENTRESTO is an ARNI indicated in adult patients for the treatment of symptomatic chronic HFrEF.1,2 ENTRESTO is not indicated for the treatment of acute HF.1,2 Patients in the PIONEER-HF/TRANSITION trial were required to be haemodynamically stabilised from an episode of ADHF while in hospital.4,11
*Defined as the decrease in eGFR of ≥35% from baseline or an increase in creatinine of ≥0.5 mg/dL from baseline and a decrease in eGFR of ≥25% from baseline at a given visit.6,8
†Primary endpoint was not met.6
‡The rates of worsening renal function, hyperkalaemia, symptomatic hypotension and angioedema did not differ significantly between the two groups. AEs that take longer to transpire may not have appeared in this study.4
§Worsening renal function was defined by an increase in the serum creatinine concentration of 0.5 mg/dL or more (≥44 μmol/L) and a decrease in the eGFR of 25% or more.4
¶The rate of permanent discontinuations due to an AE did not differ significantly between the two treatment groups.4
ACEi, angiotensin-converting enzyme inhibitor; ADHF, acute decompensated heart failure; AE, adverse event; ALT, alanine aminotransferase; AR, absolute risk; ARBs, angiotensin II receptor blockers; ARNI, angiotensin receptor neprilysin inhibitor; AST, aspartate aminotransferase; BID, bis in die (twice a day); BNP, brain natriuretic peptide; CI, confidence interval; CV, cardiovascular; Ea/Ees, ventricular-vascular coupling ratio; E/e’, ratio of early mitral inflow velocity to mitral annular early diastolic velocity; eGFR, estimated glomerular filtration rate; K+, potassium; HF, heart failure; HFrEF, heart failure with reduced ejection fraction; HR, hazard ratio; KCCQ, Kansas City cardiomyopathy questionnaire; LAVi, left atrial volume index; LV, left ventricle; LVEDVi, left ventricular end-diastolic volume index; LVEF, left ventricular ejection fraction; LVESVi, left ventricular end-systolic volume index; NT-proBNP, N-terminal-pro brain natriuretic peptide; NYHA, New York Heart Association; RAAS, renin-angiotensin-aldosterone system; RR, relative risk; NSAIDs, non-steroidal anti-inflammatory drugs; SBP, systolic blood pressure; SmPC, summary of product characteristics; Zc, impedance.
References
- ENTRESTO Summary of Product Characteristics. www.medicines.ie
- McMurray JJ, et al. N Engl J Med 2014;371(11):993–1004.
- Velazquez EJ, et al. N Engl J Med 2019;380(6):539–548.
- Velazquez EJ, et al. N Engl J Med 2019;380(6):539–548 (supplementary info).
- Desai AS, et al. JAMA 2019;322(11):1077–1084.
- Desai AS, et al. JAMA 2019;322(11):1077–1084 (supplementary info).
- Januzzi JL Jr, et al. JAMA 2019;322(11):1085–1095.
- Januzzi JL Jr, et al. JAMA 2019;322(11):1085–1095 (supplementary info).
- Ambrosy AP, et al. J Am Coll Cardiol 2020;76(9):1034–1048.
- Wachter R, et al. Eur J Heart Fail 2019;21(8):998–1007.
- Wachter R, et al. Eur J Heart Fail 2019;21(8):998–1007 (supplementary info).
- Wang Y, et al. J Am Heart Assoc 2019;8(13):e012272.
